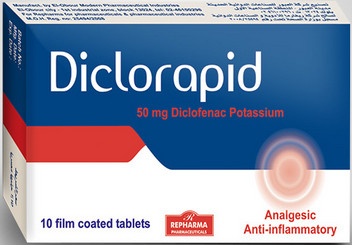
Diclorapid
Trade name :
Diclorapid.
Generic name :
Diclofenac potassium.
Composition :
Each film-coated tablet contains 50 mg of Diclofenac potassium.
In active ingredients:
Microcrystalline Cellulose ,PH 101 Lactose Magnesium Stearate, Hydroxy Propyl Methyl Cellulose ,Titanium Dioxide ,PEG 6000, Red Iron Oxide, Monohydrate, Croscarmellose Sodium.
Pharmaceutical form :
Oral film-coated tablets
– NSAIDs may cause an increased risk of serious cardiovascular thrombotic events myocardial infarction and stroke which can be fatal this risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk.
– Diclorapid (diclofenac potassium immediate-release tablets) is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery.
Description :
Diclorapid (diclofenac potassium immediate-release tablets) is a benzeneacetic acid derivative, CatafJam is available as immediate-release tablets of 50 mg (light brown) for oral administration. The chemical name is 2-[(2,6-dichlorophenyl)amino] benzeneacetc
acid, monopotassium salt.
The molecular weight is 334.25. Its molecular formula is C14H10C12NK02, and it has the following structural formula:-
The inactive ingredients in CatafJam include> Microcrystalline Cellulose ,PH 101 Lactose MagneSium Stearate, Hydroxy Propyl Methyl Cellulose ,Titanium Dioxide, PEG 6000, Red Iron Oxide, Monohydrate, Croscarmellose Sodium.
CLINICAL PHARMACOLOGY :
Pharmacodynamics
– Diclorapid (diclofenac potassium immediate-release tablets) is a nonsteroidal anti-inflammatory drug (NSAID) that exhibits anti-inflammatory, analgesic, and antipyretic activities in animal models. The mechanism of action of Diclorapid, like that of other
NSAlDs, is not completely understood but may be related to prostaglandin synthetase inhibition.
– Diclofenac is 100% absorbed after oral administration compared to IV administration as measured by urine recovery. However, due to first-pass metabolism, only about 50% of the absorbed dose is systemically available (see Table 1) .. In some fasting volunteers, measurable plasma levels are observed within 10 minutes of dosing
with Diclorapid.
– Peak plasma levels are achieved approximately 1 hour in fasting normal volunteers, and a reduction in peak plasma levels of approximately 30% .
Distribution
The apparent volume of distribution (V/F) of diclofenac potassium is 1.3 l/kg. Diclofenac is more than 99% bound to human serum proteins, primarily to albumin. Serum protein binding is constant over the concentration range (0.15-105 ?g/mL) achieved with recommended doses.
Diclofenac diffuses into and out of the synovial fluid. Diffusion into the joint occurs when plasma levels are higher than those in the synovial fluid, after which the process reverses and synovial fluid levels are higher than plasma levels. It is not known whether diffusion into the joint plays a role in the effectiveness of didofenac.
Metabolism
Five diclofenac metabolites have been identified in human plasma and urine. The metabolites include 4’·hydroxy-, 5-hydroxy·, 3’·hydroxy·, 4′,5-dihydroxy· and 3’· hydroxy-a-methoxy diclofenac. In patients with renal dysfunction, peak concentrations of metabolites 4’·hydroxy· and 5-hydroxy-diclofenac were approximately 50% and 4% of the parent compound after single oral dosing compared to 27% and 1 % in normal healthy subjects. However, diclofenac metabolites undergo further
glucuronidation and sutfation followed by biliary excretion. One diclofenac metabolite 4’·hydroxy-diclofenac has very weak phannacologic activity.
Excretion
Diclofenac is eliminated through metabolism and subsequent urinary and biliary excretion of the glucuronide and the suifate conjugates of the metabolites. little or no free unchanged diclofenac is excreted in the urine. Approximately 65% of the dose is excreted in the urine and approximately 35% in the bile as conjugates of unchanged diclofenac plus metabolites. Because renal elimination is not a significant pathway of elimination for unchanged diclofenac dosing adjustment in patients with mild to moderate renal dysfunction is not necessary the terminal half life of unchanged diclofenac is approximately 2 hours.
Special Populations
Pediatric: The pharmacokinetics of Diclorapid has not been investigated in pediatric patients.
Race: Pharmacokinetic differences due to race have not been identified.
Hepatic Insufficiency: Hepatic metabolism accounts for almost 100% of Diclorapid elimination, so patients with hepatic disease may require reduced doses of Diclorapid compared to patients with normal hepatic function .
Renal Insufficiency: Diclofenac pharmacokinetics has been investigated in subjects with renal insufficiency. No differences in the pharmacokinetics of diclofenac have been detected in studies of patients with renal impairment. In patients with renal impairment (inulin clearance 60-90, 30-60. and <30 mUmin; N=6 in each group), AUC values and elimination rate were comparable to those in heatthy subjects.
INDICATIONS AND USAGE :
Carefully consider the potential benefits and risks of Diclcrapid (diclofenac potassium immediatereleasetablets) and other treatment options before deciding to use Cataflam. Use the lowest effectivedose for the shortest duration consistent with individual patient treatment goals.
Diclorapid is indicated:
•. For treatment of primary dysmenorrhea
•. For relief of mild to moderate pain
•. For relief of the signs and symptoms of osteoarthritis
•. For relief of the signs and symptoms of rheumatoid arthritis
CONTRAINDICATIONS :
Diclorapid (diclofenac potassium immediate-release tablets) is contraindicated in patients with known hypersensitivity to didofenac. Diclorapid should not be given to patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe. rarefy fatal, anaphylactic-like reactions toNSAIDs have been reported in such patients.
Diclorapid is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery.
WARNINGS :
Cardiovascular risk:-
NSAIDS may cause an increased risk of serious cardiovascular thrombotic. events,myocardial infarction and stroke which can be fatal.This risk may increase with duration of use.patients with cardiovascular disease Or risk factors of cardiovascular disease may be at greater risk .NSAIDs is contraindicated for the treatment of pri-operative pain in the setting of coronary artery by pass graft(CABG) surgery.
Gastrointestinal Risk:-
NSAIDS cause an increased risk of serious gastrointestinal adverse events including inflammation,bleeding,ulceration and perforation of the stomach or intestine which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events.
Hypertension
events. Patients taking thiazides or loop diuretics may have impaired response to these therapies when taking NSAIDs. NSAIDs, including DicJorapid, should be used with caution in patients with hypertension. Blood pressure (BP) should be monitored closely during the initiation of NSA1D treatment and throughout the course of therapy.
Congestive Heart Failure and Edema :
Fluid retention and edema have been observed in some patients taking NSAIDs. Diclorapkf should be used with caution in patients with fluid retention or heart failure.
Renal Effects :
Caution should be used when initiating treatment with Diclorapid in patients with considerable dehydration.
Lone-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury.
Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of a nonsteroidal anti-inflammatory drug may cause a dose-dependent
reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors, and the elderly. Discontinuation of NSAID therapy is
usually followed by recovery to the pretreatment state.
Advanced Renal Disease :
No information is available from controlled clinical studies regarding the use of 9.Lclorapid in patients with advanced renal disease. Therefore, treatment with Diclorapid is not recommended in these patients with advanced renal disease. If Diclorapid therapy must be initiated, close monitoring of the patient’s renal function
is advisable.
Hepatic Effects :
Elevations of one or more liver tests may occur during therapy with Diclorapid. These laboratory abnormalities may progress, may remain unchanged, or may be transient with continued therapy.
Borderline elevations (i.e.. less than 3 times the ULN [ULN = the upper limit of the normal rangeJ) or greater elevations of transaminases occurred in about 15% of diclofenac-treated patients. Of the markers of hepatic function, AL T (SGPT) is recommended for the monitoring of liver injury.
In clinical trials, meaningful elevations (i.e., more than 3 times the ULN) of AST (GOT) (AL T was not measured in all studies) occurred in about 2% of approximately 5,700 patients at some time during diclofenac treatment. In a large, open-label, controlled trial of 3,700 patients treated for 2–6 months, patients were monitored
first at 8 weeks and 1,200 patients were monitored again at 24 weeks. Meaningful elevations of ALT and/or AST occurred in about 4% of patients and included marked elevations (i.e., more than 8 times the ULN) in about 1% of the elevations of AL T or AST was observed in patients receiving diclofenac when compared to other NSAlDs. Elevations in transaminases were seen more frequently
in patients with osteoarthritis than in those with rheumatoid arthritis. Almost all meaningful elevations in transaminases were detected before patients became symptomatic.
Abnormal tests occurred during the first 2 months of therapy with diclofenac in 42 of the 51 patients in all trials who developed marked transaminase elevations.
In postmarketing reports, cases of druq-induced hepatotoxicity have been reported in the first month, and in some cases, the first 2 months of therapy, but can occur at any time during treatment with diclofenac. Postmarketinq surveillance has reported cases of severe hepatic reactions, including liver necrosis. jaundice, fulminant
hepatitis with and without jaundice, and liver failure. Some of these reported cases resulted in fatalities or liver transplantation.
Physicians should measure transaminases periodically in patients receiving long- term therapy with diclofenac, because severe hepatotoxicity may develop without a prodrome of distinguishing symptoms. The optimum times for making the first and
subsequent transaminase measurements are not known. Based on clinical trial data and postmarketing experiences, transaminases should be monitored within 4 to 8 weeks after initiating treatment with diclofenac. However, severe hepatic reactions can occur at any time during treatment with diclofenac.
If abnormal liver tests persist or worsen, if clinical signs and/or symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophitia, rash, abdominal pain, diarrhea, dark urine, etc.), Diclorapid should be discontinued
immediately. To minimize the possibility that hepatic injury will become severe between transaminase
measurements, physicians should inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, diarrhea, pruritus, jaundice, right upper quadrant tenderness, and “flu like “symptoms), and the appropriate action patients should take if these signs and symptoms appear. To minimize the potential risk for an adverse liver related event in patients treated
with Dic1orapid, the lowest effective dose should be used for the shortest duration
Anaphylactoid Reactions :
As with other NSAIDs, anaphylactoid reactions may occur in patients without known prior exposure to Diclorapid. Diclorapid should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs.
Emergency help should be sought in cases where an anaphylactoid reaction occurs.
Skin Reactions :
NSAIDs, including Diclorapid. can cause serious skin adverse events such as exfoliative dermatitis,Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Patients should be informed about the signs and symptoms of serious skin manifestations and use of the drug should be discontinued at the first appearance
of skin rash or any other sign of hypersensitivity.
Pregnancy :
In late pregnancy, as with other NSAIDs, Diclorapid should be avoided because it may cause premature closure of the ductus arteriosus.
PRECAUTIONS :
General
Dictorapid (diclofenac potassium immediate-release tablets) cannot be expected to substitute for ccrticosteroids or to treat corticosteroid insufficiency. Abrupt discontinuation of corticosteroids may lead to disease exacerbation. Patients on prolonged corticosteroid therapy should have their therapy tapered slowly if a
decision is made to discontinue corticostercids. The pharmacological activity of Diclorapid in reducing fever and inflammation may
diminish the utility of these diagnostic signs in detecting complications of presumed noninfectious, painful conditions.
Hematological Effects
Anemia is sometimes seen in patients receiving NSAIDs, includin~ Dic1orapid. This may be due 10 fluid retention, occult or gross GI blood loss, or an Incompletely described effect upon erythropoiesis.
Patients on long-term treatment with NSAIDs, including Dlclcrapid, should have their hemoglobin or hematocrit checked if they exhibit any signs or symptoms of anemia.
NSAIDs inhibit platelet aggregation and have been shown to prolong bleeding time in some patients. Unlike aspirin, their effect on platelet function is quantitatively less, of shorter duration, and reversible.
Patients receiving Didorapid who may be adversely affected by alterations in platelet function, such as those with coaouatco disorders or patients receivinc antcoaqutants
Preexisting Asthma
Patients with asthma may have aspirin-sensitive asthma. The use of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm which can be fatal. Since cross-reactivity, induding bronchospasm, between aspirin and other nonsteroidal anti-inflammatory drugs has been reported in such aspirinasthma.
Information for Patients
Patients should be informed of the following information before Initiating
1- Diclorapid, like other NSAIDs, may cause serious CV side effects, such as MI or stroke, which may result in hospitalization and even death. Although serious CV events can occur without warning symptoms, patients should be alert for the signs Patients should be apprised of the importance this follow-up.
2- Oiclorapid, like other NSAIDs, can cause GI discomfort and, rarely, more serious GI side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Although serious GI tract ulcerations and bleeding can occur without warning symptoms, patients should be alert for the signs and symptoms of ulcerations and bleeding, and should ask for medical advice when observing any indicative sign or symptoms including epigastric pain, dyspepsia, melena, andhematemesis. Patients should be apprised of the importance of this follow-up.
3- Dccrapd. like other NSAIDs, can cause serious skin side effects such as exfoliative dennatitis, SJS, and TEN, which may result in hospitalizafons and even death. Although serious skin reactions may occur without warning, patients should be alert for the signs and symptoms of skin rash and blisters, fever, or other signs of hypersensitivity such as itching, and should ask for medical advice when observing any indicative signs or symptoms. Patients should be advised to stop the drug immediately if they develop any type of rash and contact their physicians as soon as possible.
4- Patients should promptly report signs or symptoms of unexplained weight gain or edema to their physicians.
5- Patients should be informed of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness, and “flu-like” symptoms). If these occur, patients should be instructed to stop therapy and seek immediate medical therapy.
6- Patients should be infonned of the signs of an anaphylactoid reaction (e.g., difficulty breathing, swelling of the face or throat). If these occur, patients should be instructed to seek immediate emergency help 7- in late pregnancy as with other nsaids diclorapid should be avoided because it will cause premature closure of the ductus arteriosus.
Laboratory Tests
Because serious GI tract ulcerations and bleeding can occur without warning symptoms, physicians should monitor for signs or symptoms of GI bleeding. In clinical signs and symptoms consistent with liver or renal disease oeveco. systemic manifestations occur (e.g., eosinophilia, rash, etc.) or if abnormal liver tests persist
or worsen, Diclorapid should be discontinued.
Drug Interactions :
Aspirin: When Didorapid is administered with aspirin, its protein binding is reduced. The clinical significance of this interaction is not known; however. as with other NSAIDs, concomitant administration of diclofenac and aspirin is not generally recommended because of the potential of increased adverse effects.
Methotrexate: NSAIDs have been reported to competitively inhibit methotrexate accumulation in rabbit kidney slices. This may indicate that they could enhance the toxicity of methotrexate. Caution should be used when NSAIDs are administered concomitantly with methotrexate.
Cyclosporine: Diclorapid, like other NSAIDs, may affect renal prostaglandins and increase the toxicity of certain drugs. Therefore, concomitant therapy with Didorapid
Ace inhibitors: this interaction should be used when Didorapid
ACE Inhibitors: Reports suggest that NSAIDs may diminish the antihypertensive effect of ACE inhibitors. This interaction should be given consideration rn patients taking NSAIDs concomitantly with ACE inhibitors.
Furosemide: Clink;al studies, as well as postmarketing observations, have shown that Oiclorapid can reduce the natriuretic effect of furosemide and thiazides in some patients. This response has been attributed to inhibition of renal prostaglandin synthesis. During concomitant therapy with NSAlDs, the patient should be observed carefully for signs of renal failure.
Lithium: NSAIDs have produced an elevation of plasma lithium levels and a reduction in renal lithium clearance. The mean minimum lithium concentration increased 15% and the renal clearance was decreased by approximately 20%. These effects have been attributed to inhibition of renal prostaglandin synthesis by
the NSAID. Thus, when NSAlDs and lithium are administered concurrently, subjects should be observed carefully for signs of lithium toxicity.
Warfarin: The effects of warfarin and NSAIOs on GI bleeding are synergistic, such that users of both drugs together have a risk of serious GI bleeding higher than users of either drug alone.
Pregnancy :
Teratogenic Effects: Pregnancy Category C :
Reproductive studies conducted in rats and rabbits have not demonstrated evidence of developmental abnormalities. However, animal reproduction studies are not always predictive of human response. There are no adequate and well-controlled studies in pregnant women. Nonteratogenic effects : because of the known effects of nonsteroidal anti-inflammatory drugs on the fetal cardiovascular system (dosure of ductus arteriosus), use during pregnancy (partiaJlarty late pregnancy) should be avoided.
Labor and Delivery :
In rat studies with NSAIDs, as with other drugs known to inhibit prostaglandin synthesise women are unknown.
Nursing Mothers :
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Diclorapid, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use :
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use :
As with any NSAIDs, caution should be exercised in treating the elderly (65 years and Older).
ADVERSE REACTIONS :
In 718 patients treated for shorter periods, i.e., 2 weeks or less, with Catafiam® (diclofenac potassium immediate-release tablets), adverse reactions were reported one-half to one-tenth as frequently as by patients treated for longer periods. In a 6-month, double-blind trial comparing CataHam (N=196) versus Voltaren® (diclofenac sodium delayed-release tablets) (N=197) versus ibuprofen (N=197), adverse reactions were similar in nature and frequency. occurring in approximately 1 %-1 0% of patients are: In patients taking Cataflam or other NSAlDs, the most frequently reported adverse
experiences Gastrointestinal experiences including: abdominal pain, constipation, diarthea. dyspepsia, flatulence, gross bleeding/perforation, heartburn, nausea, GI ulcers
(gastric/duodenal) and vomiting.
Abnormal renal function, anemia, dizziness, edema, elevated liver enzymes, headaches, increased bleeding time, pruritus, rashes and tinnitus. Additional adverse experiences reported occasionally include:
Body as a Whole: fever, infection, sepsis.
Cardiovascular System: congestive heart failure, hypertension, tachycardia, syncope.
Digestive System: dry mouth, esophagitis, gastric/peptic ulcers, gastritis, gastrointestinal bleeding, glossitis, hematemesis, hepatitis, jaundice
Hemic and Lymphatic System: ecchymosis, eosinophilia, leukopenia, melena, purpura, rectal bleeding, stomatitis, thrombocytopenia.
Metabolic and Nutritional: weight changes.
Nervous System: anxiety, asthenia, confusion, depression, dream abnormalities, drowsiness, insomnia, malaise, nervousness, paresthesia, somnolence, tremors, vertigo
Respiratory System: asthma, dyspnea.
Skin and Appendages: alopecia, photosensitivity, sweating increased.
Special Senses: blurred vision.
Urogenital System: cystitis, dysuria, bereatutia. interstitial nephritis, oliguria/JX)Iyuria, proteinuria, renal failure.
Other adverse reactions, which occur rarely are:
Body as a Whole: anaphylactic reactions, appetite changes, death.
Cardiovascular System: arrhythmia, hypotension, myocardial infarction, palpitations, vasculitis
Digestive System: colitis, eructation, liver failure, pancreatitis.
Hemic and Lymphatic System: agranulocytosis, hemolytic anemia, aplastic anemia,
Nervous System: convulsions, coma, hallucinations, meningitis.
Respiratory System: respiratory depression, pneumonia.
Skin and Appendages: angioedema, toxic epidennal necrolysis, erythema multifonne, exfoliative dermatitis, Stevens-Johnson syndrome, urticaria
Special Senses: conjunctivitis, hearing impainnent.
OVERDOSAGE :
Symptoms following acute NSAID overdoses are usually limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which are generally reversible with supportive care. Gastrointestinal bleeding can occur. Hypertension, acute renal failure, respiratory depression and coma may occur, but are rare. Anaphylactoid
reactions have been reported with therapeutic ingestion of NSAIDs, and may occur following an overdose. Patients should be managed by symptomatic and supportive care following an NSAID overdose. There are no specific antidotes. Emesis and/or activated charcoal
(60 to 100 g in aduns. 1 to 2 g/kg in children) and/or osmotic cathartic may be indicated in patients seen within 4 hours of ingestion with symptoms or following a large overdose (5 to 10 times the usual dose). Forced diuresis, alkalinization of urine, hemodialysis, or hemoperlusion may not be useful due to high protein binding.
DOSAGE AND ADMINISTRATION :
Carefully consider the potential benefits and risks of Didoraptd (diclofenac potassium immediaterelease tablets) and other treatment options before deciding to use Diclorapid. Use the
lowest effective dose for the shortest duration consistent with individual patient treatment goals (see WARNINGS).
After observing the response to initial therapy with Diclorapid, the dose and frequency should be adjusted to suit an individual patient’s needs.
For treatment of pain or primary dysrnenorrnea the recommended dosage is 50 mg
For the relief of osteoarthritis the recommended dosage is 100-150 mglday in divided
Package & Storage :
1,3 strips of 10 film-coated tablets.
Store below 30°C at a dry place.
Keep out of reach of children.
Produced by :
Meivo International for Pharmaceutical lndustries
